MEDtube is the largest social eLearning platform for 350,000+ professionals sharing 30,000+ videos, courses, images, documents and webinars
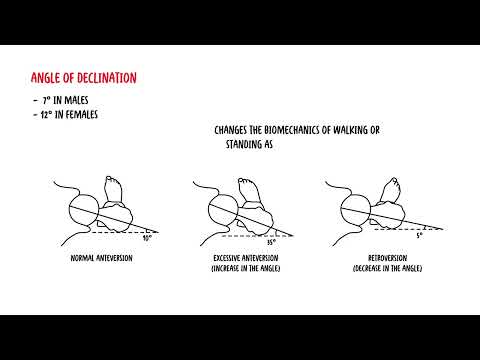
Register for freeFemur clinical anatomy
Dive deep into the world of human anatomy with our latest video on the femur. What You'll Learn: -The Femur Unveiled: Get up close and personal with the anatomy of the femur, exploring its structure,...
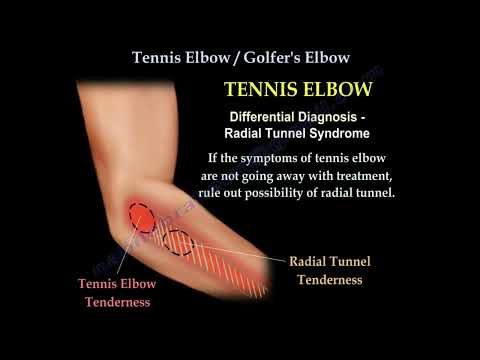
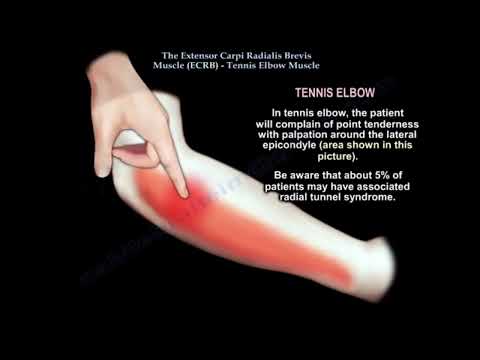
Tennis Elbow - Anatomy & Treatment
Tennis Elbow (lateral epicondylitis) usually occurs in patients who perform manual labor or sports which require twisting and extension of the wrist against.
Tennis Elbow Clinical and Anatomical Considerations
Tennis Elbow (lateral epicondylitis) is an overuse injury that causes inflammation, tendinosis and lateral elbow pain at the origin of a small muscle called the extensor carpi radialis brevis (ECRB).
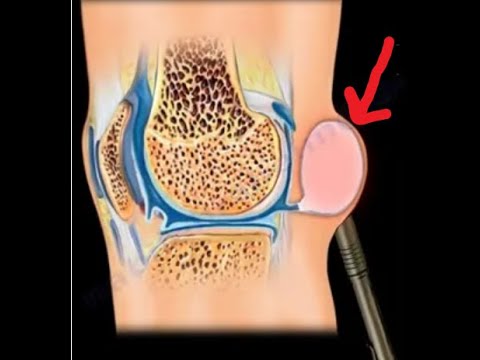
Baker's Cyst- Relationship to Meniscus Tears...
A Baker's cyst is a benign swelling found posterior to the medial femoral condyle. Knee effusion or swelling from intra-articular pathology allows the fluid to go through the valve to the cyst in one...
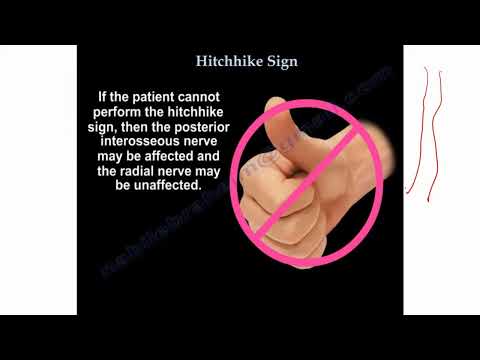
Common Nerve Conditions of the Upper Extremity
This video provides a concise review of common nerve conditions of the upper extremity.
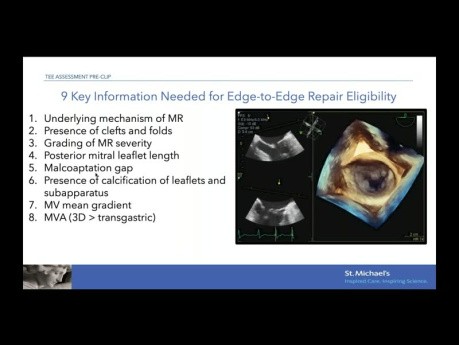
Echocardiographic Evaluation for Mitral Edge-to-Edge...
Echocardiographic evaluation for mitral edge-to-edge repair.
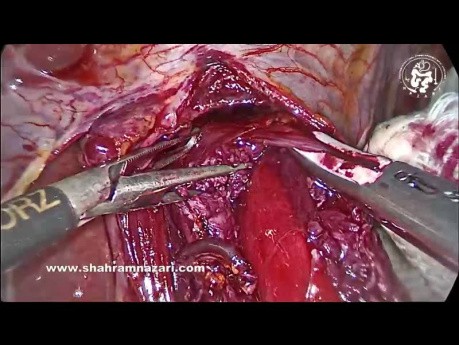
Technique of Heller Myotomy for Achalasia
Surgical video case: the easiest place to start the myotomy is on the distal esophagus 1-1.5 cm above GEJ. Grasp the 2 sides of the muscularis, folding the muscle into the jaws of the graspers. By streching...
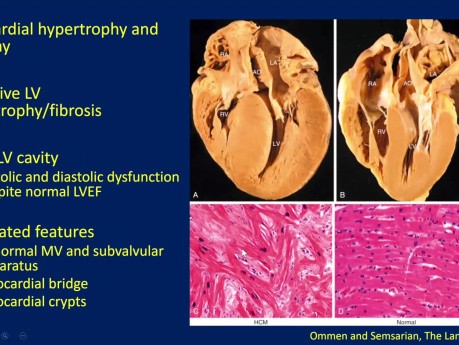
Echocardiographic Evaluation of Hypertrophic...
Echocardiographic evaluation of hypertrophic cardiomyopathy (HCM). Date: January 18, 2024 Speaker: Sean Cai MD FRCPC, Echo Fellow, St. Michael's Hospital. Objectives: 1. Understand basic pathophysiology...
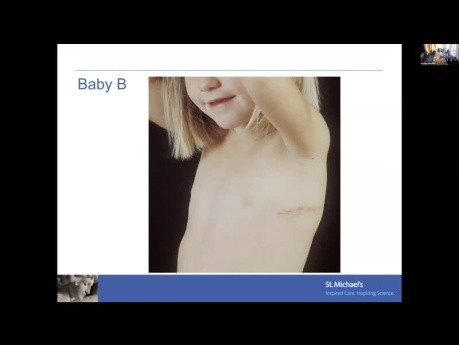
Aortic Valve Disease Across the Ages
Aortic valve disease across the ages. Date: February 29, 2024. Speaker: Dr. Ra Han, Pediatric Cardiologist, St. Michael's Hospital Objectives: 1. Appreciate the impact of aortic valve stenosis on the...
Funky Motion: Basic and Advanced Wall Motion...
Funky motion: basic and advanced wall motion interpretation in echocardiography. Date: Thursday, 11 Jan 2024. Speaker: Howard Leong-Poi MD FRCPC Echocardiographer & Cardiologist, St. Michael's Hospital...
External Fixation
External Fixation (OrthoConcepts). Join the channel membership to unlock access to premium courses https://www. youtube.com/channel/UCpKGX6esbmV364XDaTQGckQ/join
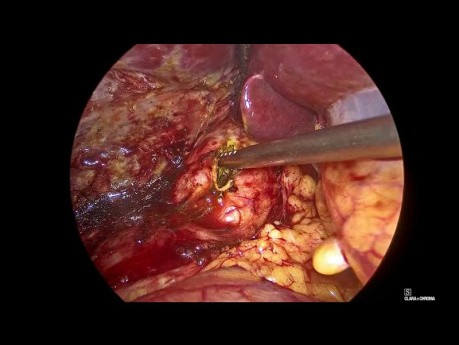
Laparoscopic Common Bile Duct Exploration and...
Laparoscopic video case: this a cae of 52 year old female presented with abdominal pain and discomfort, laparoscopic cholecystectomy done 5 years back. Investigations revealed cbd calculi with concomitant...
Featured channels
Mitral Valve Repair Center at The Mount...
As one of the world's most respected and experienced heart…
EUS - ENDO
EUS-ENDO will offer one day of live transmission from Paoli-Calmettes…
SAGES - Society of American Gastrointestinal...
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) is…