How to Reduce a Shoulder Dislocation | How to Pop Your Shoulder Back in Place
Case description
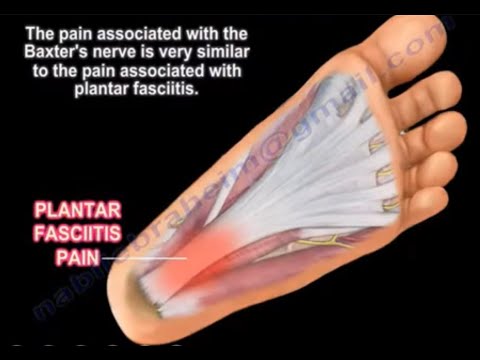
-Crepitus/Instability
- Ecchymosis
- Humeral neck/shaft fracture
- Clavicle fracture
- Posterior dislocation
- Luxatio erecta
- C-spine injury
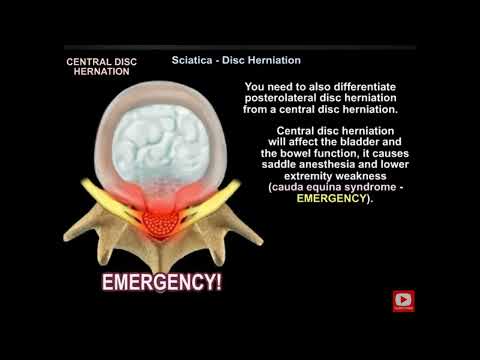
When deciding when to reduce the shoulder, you decide if the dislocation is anterior, posterior, or inferior. If you have a posterior or inferior dislocation we recommend that you assess the situation for any neurovascular compromise and refer them immediately to the emergency department.
For an anterior dislocation, if the patient is over the age of 40 we recommend that you assess immobilize and refer them to the emergency room due to the likelihood of a clinically significant fracture. If the patient is under the age of 40, you must further assess their neurovascular compromise. If there is any indication for a neurovasuclar compromise, we recommend that you give one attempt and then weather or not they are reduced after that attempt, you would recess, immobilize and send to the emergency room. Once the shoulder is reduced, we recommend the patient go see an orthopedic surgeon.
Why reduce a shoulder dislocation? Early reduction may minimize progression of injury, minimize stretch/compression of neurovascular structures,, minimize muscle spasms and minimize humeral head defects in locked dislocations. This also decreases the time in the emergency department and the cost.
The best case scenario is:
- Patient consent to treat
- Patient in a sports medicine facility
- Table present (easier than a sideline bench)
- Patient is relaxed/comfortable as possible
- Reduction technique within level of comfort
- Early reduction accomplished
The most common shoulder dislocation techniques is the hippocratic technique. The milch technique involves the patient lying supine on the table. The clinician places one hand over the humeral head. the patient's hand is placed behind their head either actively or passively. This technique has a 72-89% success rate with the first attempt.
The next method is the external rotation technique. The patient lies supine. The elbow is flexed at 20 degrees. The clinician slowly externally rotates the shoulder. Reduction is commonly achieved between 70-110 degrees of external rotation. This method has an 89% success rate on the first attempt.
The traction-counter traction technique involves the patient lying supine. Clinician one pulls traction using a sheet or towel. The patient's arm is placed in 90 degrees of abduction and 90 degrees of external rotation. Clinician two pulls traction perpendicular to the patient's body.
The scapular manipulation technique involves the patient lying supine. Gentle weight up to 15 lbs is attached to the patient's wrist. Clinician manually rotates inferior angle of the scapula medially. This technique has a 92% success rate.
Stimpson technique, also known as the hanging arm method, involves the patient lying prone with the injured arm slightly abducted over the table. The clinician applies gentle traction or a weight. This method has a 96% success rate with combined scapular manipulation.
Once the shoulder has been reduced, you reassess the neurovascular status and ROM/strength. You immobilize the arm, document and possibly refer for diagnostics.
This user also sharing
Recommended
OrthoNews - Frozen Shoulder
Orthopaedic Academy
views: 338
Explaining Low Back Pain
Nabil Ebraheim
views: 440