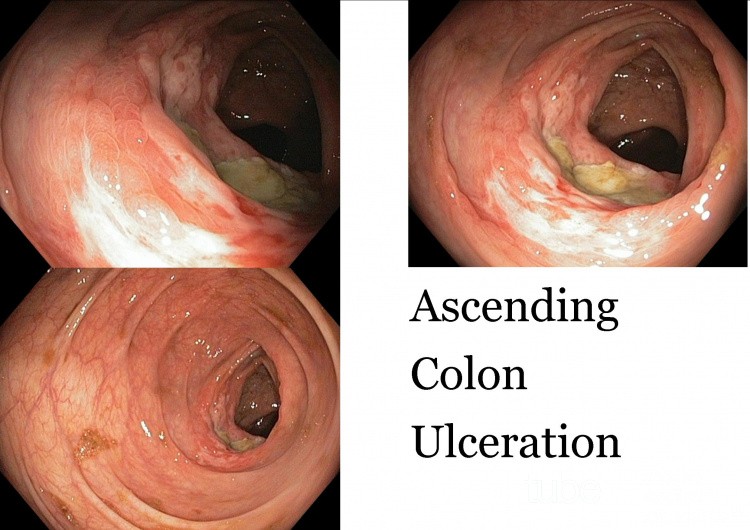
Ascending Colon Ulceration
Case description
Pt has a BMI of 33 and is Hypertensive with no other significant medical/surgical or Family history.
He is seen by the doc on call, who felt it might be appendicitis, he is worked up sent for CT scan and I am asked to consult afterwards.
At the time when the primary physician saw the patietn, he was asymptomatic and pain free after IVI fluids and IV Ketorolac. Vitals normal. (about 48 hours since initial symptom onset.
Laboratory investigations:White cell count of 10.8, hemoglobin
141, platelet count 270, (Initial white cell count upon presentation to ER was 14.1)
LFT Lipase Lytes Renal Function, Abd-Xray etc all normal. CRP 36.
Ct Abdomen:Revealed Mild inflammatory stranding of the mesenteric fat along the lateral aspect of the mid ascending colon. Radiologists differential is Colitis vs epiploic appendagitis.
Clinically felt this was likely Inflammatory Bowel disease or Ischemic colitis, pt is booked for a colonoscopy.
Colonoscopy:
This lesion in seen in the mid ascending Colon a week later, Several biopsies with a large biopsy forceps, the lesion was HARD and due to that, the lesion was suspicious of Cancer
Pathology:
Colon, ascending, lesion, biopsies:
- ACTIVE CHRONIC ULCERATION, NON-SPECIFIC, PLEASE SEE MICROSCOPIC REPORT.
MICROSCOPIC DESCRIPTION
This patient's Netcare file has been reviewed and his history of recent abdominal pain with
diarrhea, CT evidence of inflammatory stranding of mesenteric fat along the lateral aspect
of the mid ascending colon and colonoscopy finding of a 3 cm long flat lesion spanning 70%
of the circumference of the mid ascending colon is noted.
Microscopic examination of seven levels through specimen B1 and two through specimen B2
reveal the presence of a large ulcer. The ulcer base consists of acute and chronic
inflammatory granulation tissue with fibrosis. The inflammatory reaction is dominated by
neutrophils with smaller numbers of lymphocytes, eosinophils and macrophages. The adjacent
mucosa shows mild distortion of crypt architecture and an increase in the numbers of lamina
propria, eosinophils and lymphocytes.
There is no microscopic evidence of carcinoma, or other neoplasm.
No evidence of helminths, helminth eggs, amoeba, foreign bodies, viropathic changes,
granulomatous inflammation, hemosiderin, diverticulum, ectopic tissue or herniation is
noted.
Characteristic features of ischemia such as extensive mucosal hemorrhage, necrosis, atrophy
or hemosiderin deposition are absent.
There is no marked crypt distortion, intramucosal granulomata, fissures, fistula or other
features of inflammatory bowel disease.
The multifocal superficial intense acute inflammation usually seen with clostridium
difficile is absent.
The inflammation within the mucosa which is present is non-specific in type.
In summary, the microscopic findings within this ulcer are non-specific. Possible causes
include drugs such as NSAID analgesics, stercoral ulceration or an unusual manifestation of
inflammatory bowel disease or ischemia.
If clinical suspicion of malignancy remains high, additional sampling of other portions of this lesion is recommended.
Other photos of this user
Serrated adenoma
American Association for Primary Ca…
views: 4530
Serrated Adenoma
American Association for Primary Ca…
views: 5924
Recommended
Portal Venous Gas
Noll Jan-Philip
views: 527
Autoimmune Hepatitis
Armando Hasudungan
views: 944
Multiple Stone CBD ERCP Clearance
Adrian Wróżek
views: 884