MEDtube is the largest social eLearning platform for 350,000+ professionals sharing 30,000+ videos, courses, images, documents and webinars
Register for freeBronchial Wash
This video is presenting how to perform a bronchial wash with a single-use bronchoscope. The successful miniaturisation of Broncoflex has resulted in a large working channel in a medium-sized scope, supporting...
Donation After Cardiac Death
Professor Zeraatian's research on donation after cardiac death (DCD) illuminates a critical aspect of organ transplantation. His work delves into the ethical considerations, medical protocols, and logistical...
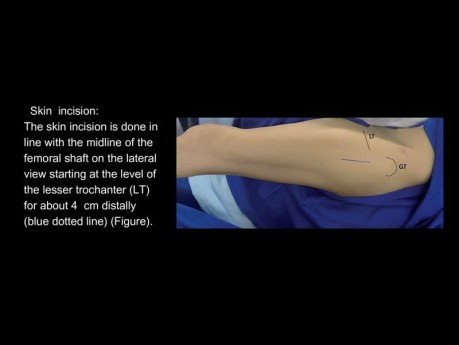
Chronic Rhinosinusitis with Polyps - Fullhouse...
Chronic Rhinosinusitis with Polyps - Fullhouse FESS. By Xavier Gonzalez-Compta MD, PhD at VII Hands on FESS course EENS Barcelona 2017.
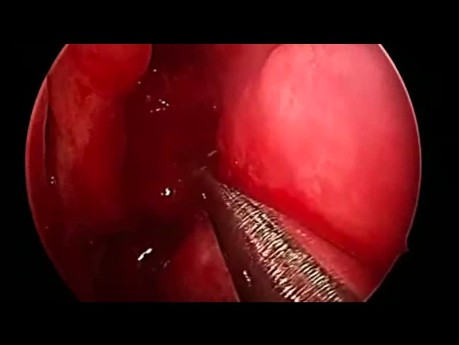
Ectopic Pregnancy
Video case: 11 weeks pregnant lady completely asymptomatic came few days before her formal dating scan for just routine check up.
Biomechanics of Fracture Fixation
Biomechanics of fracture fixation. Join the channel membership to unlock access to premium courses https://www.youtube. com/channel/UCpKGX6esbmV364XDaTQGckQ/join
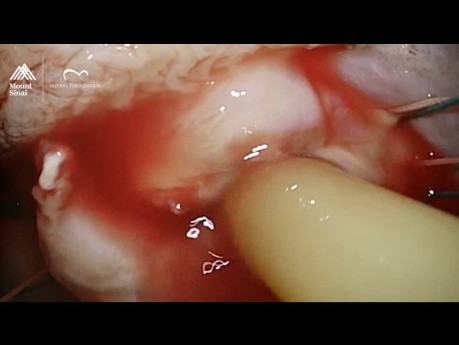
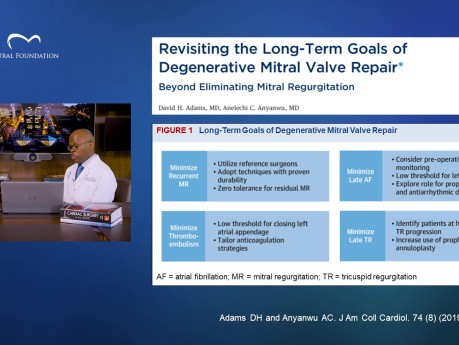
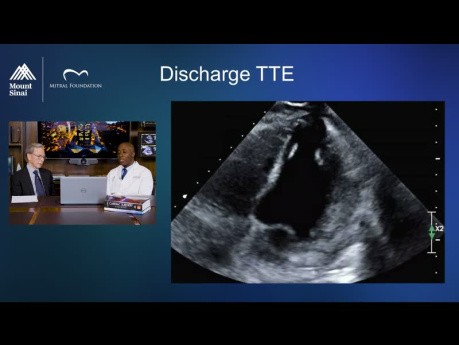
Mitral Valve Repair for Native Mitral Valve Endocarditis...
Reviewing surgical video from a case study, we explore the complexity of diagnosing mitral valve endocarditis, especially when there is a risk of embolism. In this discussion, we review: ● The key role...
Risk Factors for Sudden Cardiac Death from Arrhythmic...
Arrhythmic mitral valve prolapse has been identified as a potential cause of sudden cardiac death among some patients with primary mitral regurgitation. What are critical indications and possible mechanisms?...
Treating Secondary Mitral Valve Regurgitation...
Secondary mitral valve regurgitation increases the dangers of heart failure, and the two conditions are often encountered together. In this discussion, we highlight: ● The destructive feedback loop between...
Why Mitral Valve Repair Surgery is the Safest...
In this discussion, we review a six-year study of over 53,000 patients that reveals the extraordinary safety and durability of mitral valve repairs among patients with primary mitral regurgitation. We...
Left Ventricular Pseudoaneurysm: A Surprising...
In this video, we review a challenging case of a 48-year-old woman presenting with chest pain. We explore the role of Echo, CT, and MRI imaging, and highlight how surprising and dramatic results led to...
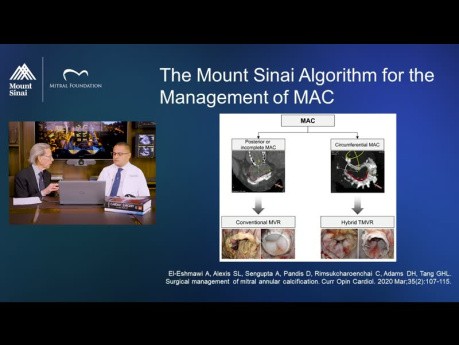
Mitral Annular Calcification (MAC): An Algorithmic...
Mitral Annular Calcification (MAC) is a complex and increasingly common syndrome. In this discussion, we review Mount Sinai’s proven algorithm for determining the best treatment for MAC, as well as imaging...
Featured channels
Mitral Valve Repair Center at The Mount...
As one of the world's most respected and experienced heart…
EUS - ENDO
EUS-ENDO will offer one day of live transmission from Paoli-Calmettes…
SAGES - Society of American Gastrointestinal...
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) is…